by Raven Health | Nov 20, 2025 | Blogs

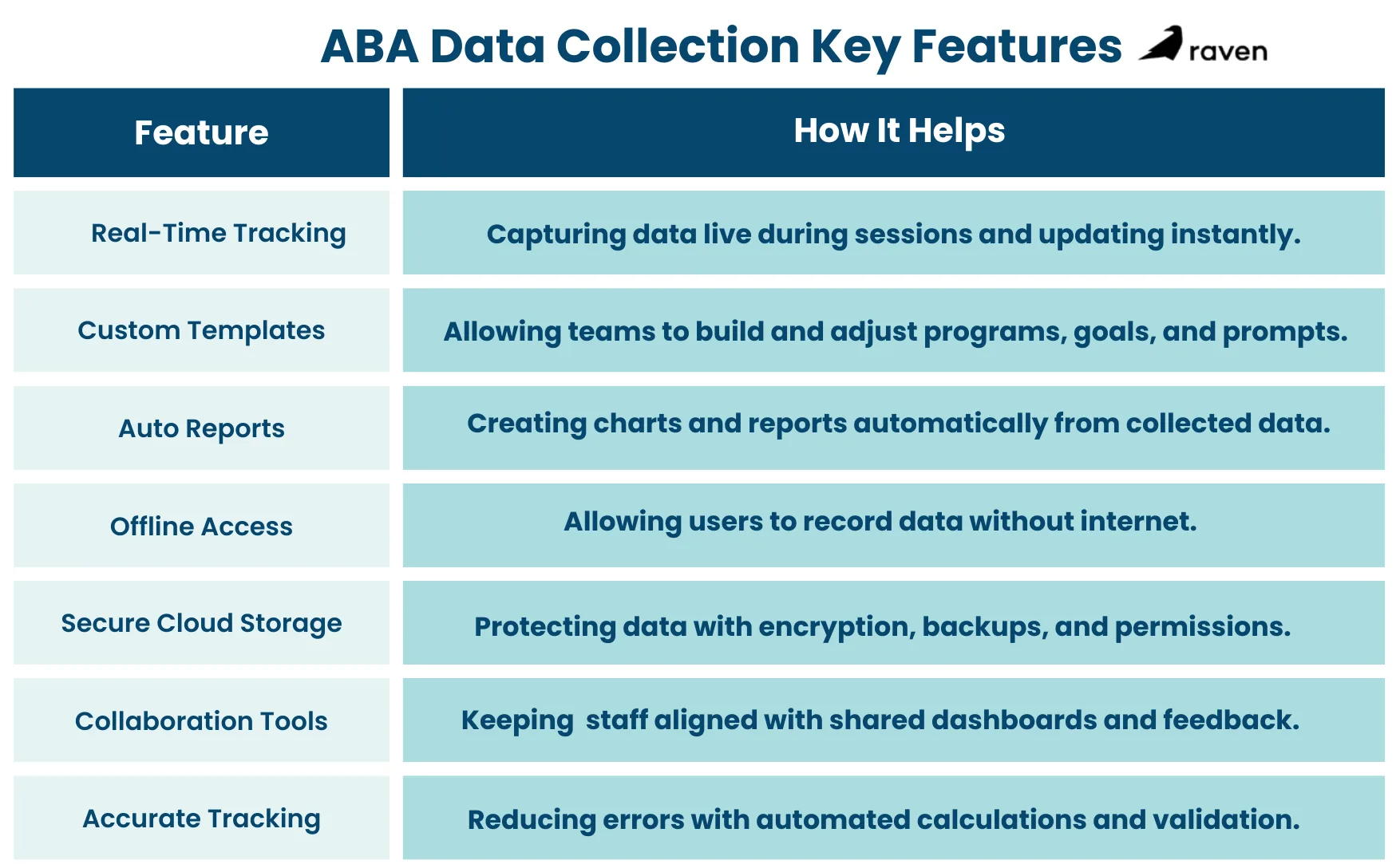
ABA data collection software turns complex therapy records into clear insights. Therapists need to gather accurate information about behaviors and skills. Good software helps teams log session data quickly, so they can adjust treatment and see real progress.
Studies show that clinics using consistent digital data collection make 35% faster progress toward goals than those relying on manual methods. In this article, you will explore the top features to look for in ABA data collection software.
1. Real-Time Data Tracking and Entry
Live Session Recording
The best ABA apps let staff record data during therapy sessions on tablets or phones. This way, behaviors and trials are logged as they happen, not hours later from memory. A mobile app with auto-sync ensures no data is lost and that supervisors see updates right away.
Immediate Syncing
When data syncs in real time, BCBAs can access fresh information instantly. Real-time tracking frees clinicians from jumping between disjointed charts and saves time so they can focus on clients. This instant data flow helps teams spot issues quickly and adjust plans on the spot.
Accurate Behavior Logs
Entering data as it occurs cuts down errors, and digital timers and counters automatically calculate duration or frequency. This approach helps keep every data collection method consistent across staff and sessions, ensuring accuracy because even small mistakes can skew treatment decisions.
2. Customizable Programs and Templates
Editable Data Fields
It’s essential for ABA software to empower therapists to create fully customizable program templates. Clinicians can set up goal-specific data forms and fields for each child’s needs. For example, they can define unique prompts and goal steps in the system. This flexibility means the software fits the therapy, not the other way around.
Behavior and Skill Templates
Many platforms include built-in tools for common ABA program types. Users can generate templates for things like discrete trial training or preference assessments and adapt them to each case. This avoids recreating forms from scratch and keeps data collection consistent.
Integrated Session Notes
Custom program templates often tie into note-taking features. Providers can attach instructions or criteria to each data field. This ensures any therapist using the program knows exactly what to do and how to score each trial. Over time, having precise, standardized templates helps supervisors check consistency across staff.
3. Automated Reporting and Progress Visualization
Auto-Generated Reports
Good ABA data collection software can build progress reports and charts at the push of a button. Instead of manually compiling graphs, the system pulls together all the data for each goal. AI-powered tools can even auto-write session summaries that align with insurance requirements, saving clinicians hours of paperwork.
Built-in Charting
Software usually includes graphing tools that update as new data comes in. For example, one platform offers up to 20 customization options for progress graphs, you can add trend lines, split data by therapist, compare conditions, and more. These visual charts make it easy to see if a child is making gains or needs extra help.
Export and Review
It should be easy to export data and reports (PDF, CSV, etc.) for review outside the app. These visual reports help therapists, supervisors, and families understand progress without reading raw spreadsheets. Having ready-made graphs and summaries means everyone can stay informed at a glance.
Goal Mastery Features
Some software even automates mastery criteria. Clinicians can set targets (like “90% correct over three sessions”), and the system will flag or master out a skill once met. This automatic progress tracking cuts down on manual checks and ensures goals are updated promptly.
4. Offline Data Entry and Mobile Access
Offline-Mode
Therapists often work where the internet is spotty. Leading ABA apps let them record data offline and sync later. The app stores entries securely on the device until Wi-Fi returns. This way, a session isn’t interrupted by a network glitch, and once online, the data updates automatically, so nothing is lost.
Cross-Device Flexibility
Quality ABA software works on phones, tablets, and computers. Whether staff bring an iPad or a laptop, data goes into the same cloud system. This flexibility lets clinicians choose the device they’re comfortable with and ensures the entire team always sees the latest data.
Data Security Offline
Even in offline-mode, data stays encrypted on the device. When syncing later, it moves to the cloud over an encrypted connection. This protects client privacy without sacrificing the convenience of mobile data entry.
5. Secure Cloud Storage and Data Security
HIPAA-Compliant Cloud
All client data should be encrypted and stored on secure cloud servers. Reputable ABA software meets HIPAA standards, using encryption and access controls to safeguard information. This not only protects records but also ensures clinics stay compliant with privacy laws. (For example, one case study highlights how secure cloud storage reduced data loss for a clinic.)
Automatic Backups
Cloud-based systems automatically back up data, reducing the risk of loss if a device breaks or a file is deleted. Daily or real-time backups mean you don’t have to worry about losing months of data to a computer crash. One ABA platform even notes that secure cloud storage cuts down data loss dramatically.
User Permissions
Good ABA tools let administrators assign roles (BCBA, RBT, admin, etc.), so each team member sees only what they need. Audit logs track who entered or changed data, adding transparency. These security features help supervisors trust the data and protect sensitive client information.
6. Supervision and Collaboration
Shared Dashboard
Supervisors and team members work from one central database. A shared dashboard or client portal means therapists, BCBAs, and even parents can view the same data.
Real-Time Oversight
Because data is entered live, supervisors can review session data quickly. Clinical leads can monitor progress during or right after sessions. This immediate feedback helps them coach staff and ensure data quality in real time.
Built-In Communication
Many platforms include tools for notes or comments. Supervisors can add feedback directly in a session report, or therapists can flag unusual incidents. Keeping these messages linked to the client’s record avoids miscommunication. It’s like having a built-in chat about the data so nothing falls through the cracks.
Family Involvement
Sharing progress with parents improves collaboration. Some software lets providers share read-only reports or charts with families. When parents see clear evidence of success (or challenges), they can help reinforce skills at home. In this way, data collection becomes a team effort supporting the child.
7. Ensuring Accurate, Efficient Tracking
Error Reduction
Digital data entry dramatically cuts human mistakes. One ABA practice reported doubling data accuracy after switching from paper. On a digital form, counts and times add up automatically, and drop-down choices keep entries standardized. This means the data your team relies on is far more likely to be correct.
Consistent Measurement
The software enforces consistent methods (e.g., all staff use the same behavior definitions and units). This consistency is crucial for comparing data across sessions or staff members. If everyone records data the same way, progress graphs are reliable, and no one needs to second-guess whether a change in numbers is real or just an input error.
Built-In Calculations
Leading tools auto-calculate rates, percentages, and other metrics. For example, you might just enter trial outcomes, and the system shows you the percentage correct instantly. This saves time and keeps the team on task, rather than scrambling with calculators during a session.
Quick Alerts
Look for software that can flag data trends. For instance, if a child’s performance suddenly dips or if data hasn’t been entered for a while, the system can alert supervisors. These proactive checks help catch issues early and keep interventions on track.
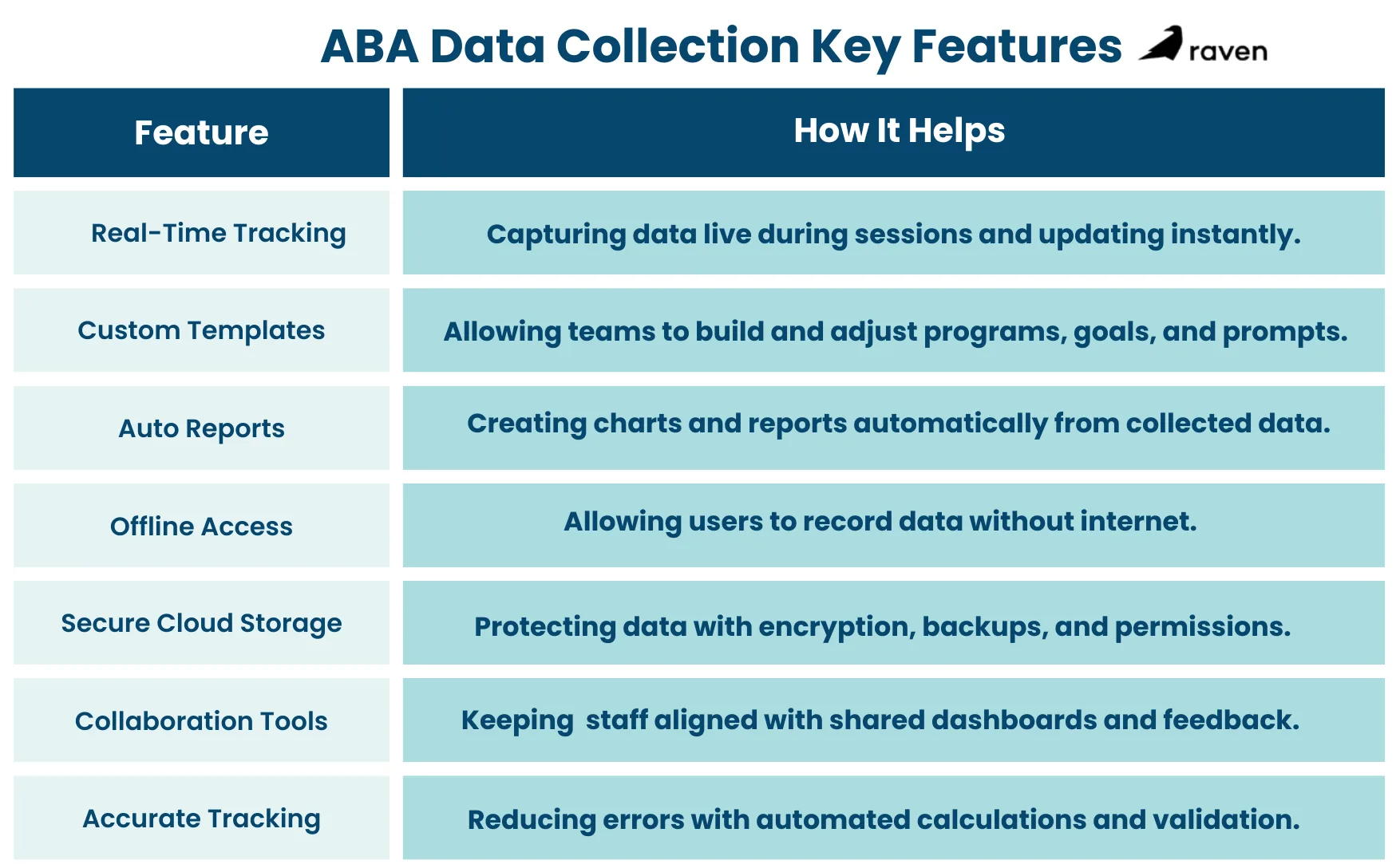
Conclusion
Choosing the right ABA data software means weighing these features carefully. Look for tools that support live data entry, flexible program templates, automatic reporting with visual charts, offline/mobile access, and robust security. These capabilities not only save therapists time but also ensure every data point is reliable. They turn raw numbers into clear insights, driving better care.

by Raven Health | Nov 19, 2025 | Blogs

Momentary Time Sampling (MTS) is a practical method for collecting behavioral data in Applied Behavior Analysis. It tells you whether a target behavior may be happening at specific moments rather than recording everything that happens across an entire observation period.
This makes MTS fast, reliable for trends, and especially useful in group or busy settings. In this article, you will explore more about MTS, know how it differs from partial and whole interval recording, and learn its uses in ABA.
What is Momentary Time Sampling?
Momentary Time Sampling is a data collection method that involves observing at predetermined moments and recording whether the behavior is present exactly at that instant.
It works in the following ways:
- You divide an observation session into equal-length intervals (for example, twenty 30-second intervals during a 10-minute observation).
- At the end (or start) of each interval, you look up and mark whether the behavior is occurring at that moment.
- Count the number of “yes” checks and divide by total moments observed to get a percentage (moments with behavior ÷ total moments × 100).
MTS will provide you with a snapshot series, many quick photos of behavior across time, rather than a continuous movie, making it a practical tool for ABA data collection.
How to Conduct a Momentary Time Sampling Session?
Define the behavior clearly
Make it observable and measurable. For example: On-task behavior = eyes on work and hands engaged with materials.
Choose observation length and interval
Common choices include 10–30 minutes total and intervals of 15–60 seconds. Shorter intervals catch faster behaviors better. For example: 10 minutes with 20 thirty-second intervals.
Decide the moment to observe
Most practitioners use the end of each interval (e.g., at 0:30, 1:00, 1:30). This is simple and consistent.
Use a timer or app
Set an audible timer or an interval timer app that beeps at each moment to mark.
Record at each moment
Mark “1” if the behavior is present at the instant, “0” if not.
Calculate percent occurrence
% = (number of yes marks / total intervals) × 100.
Check reliability
Have a second observer collect data simultaneously during at least some sessions to compute Interobserver Agreement (IOA).
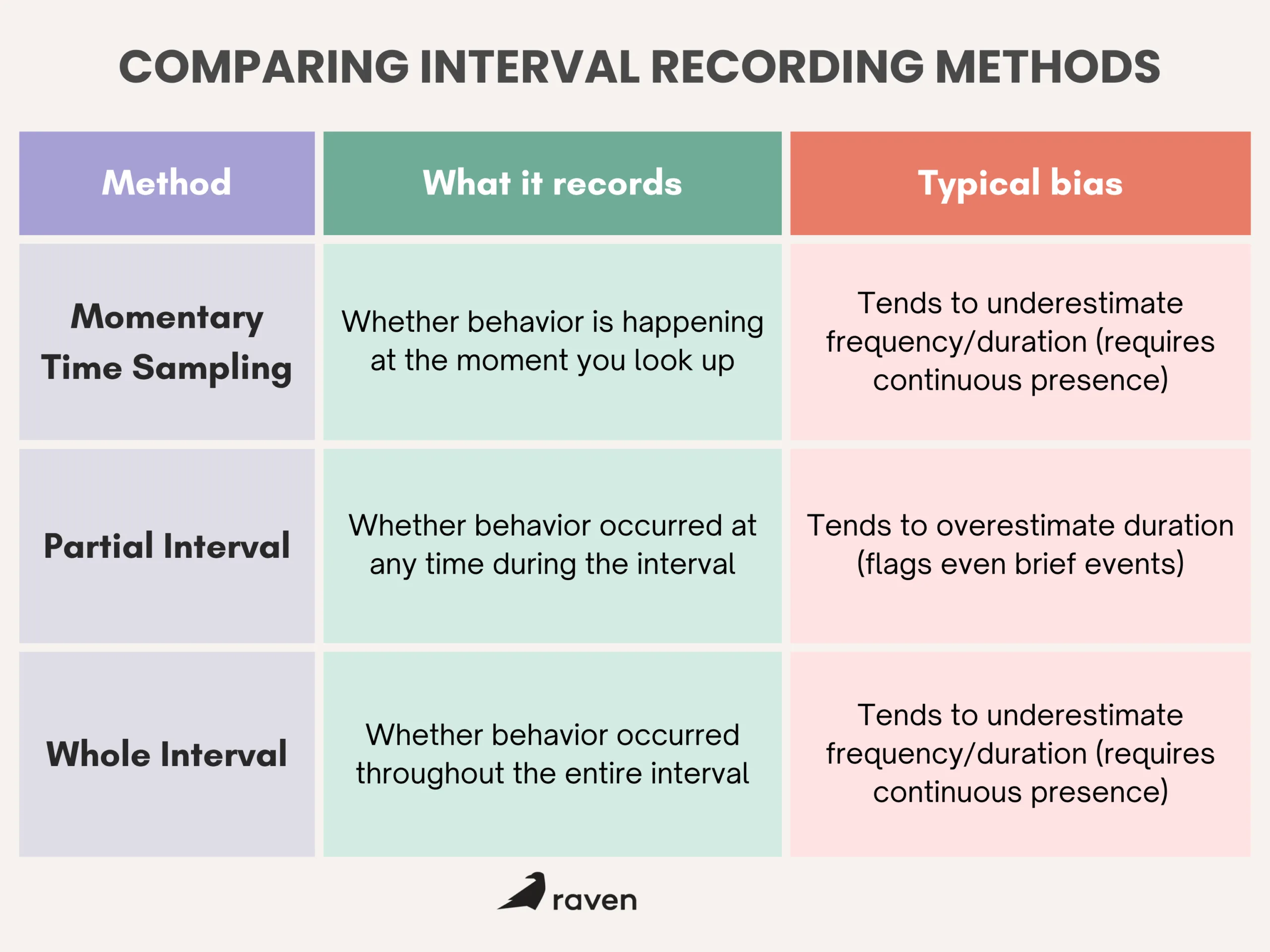
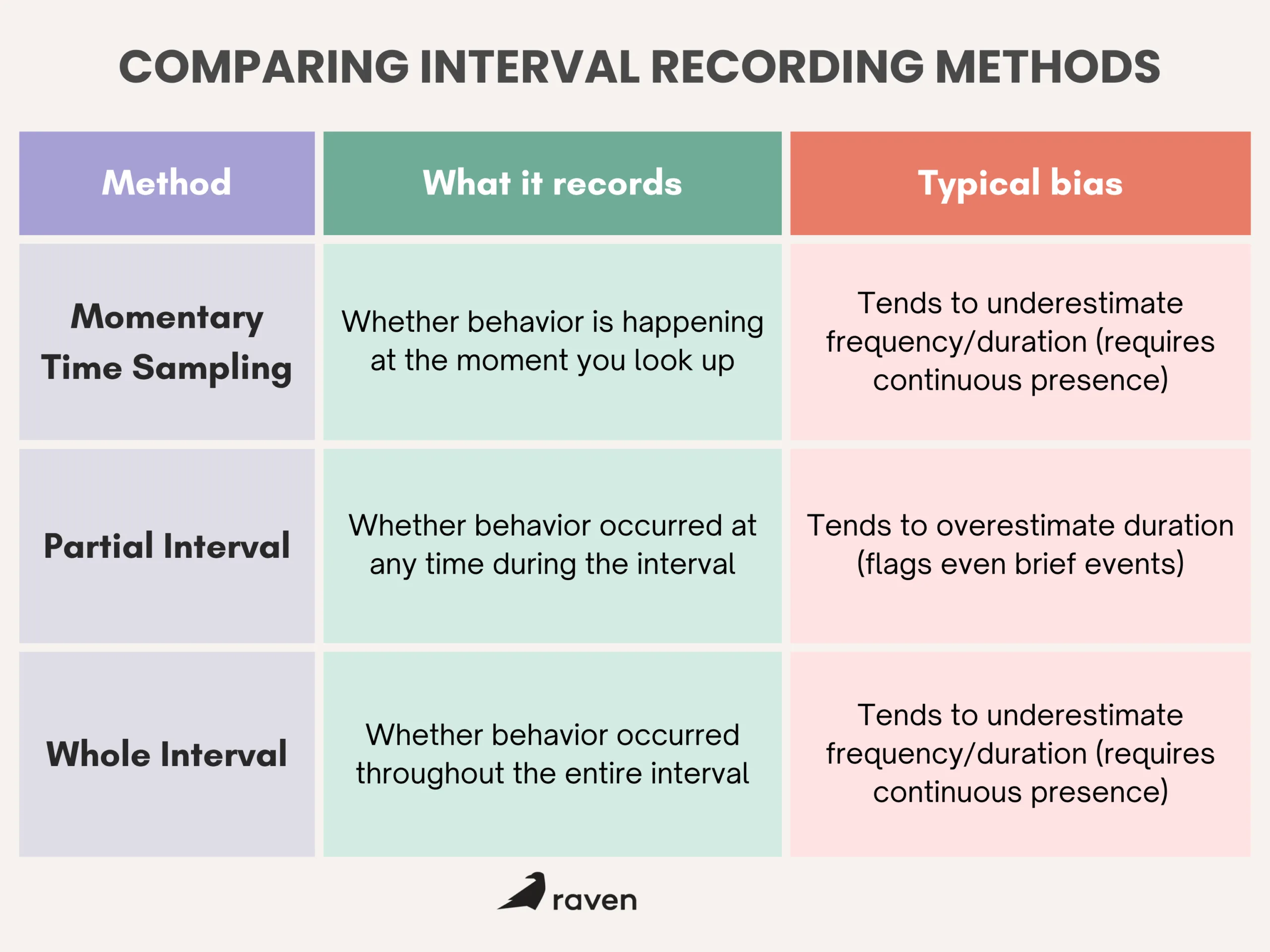
How MTS Differs from Partial and Whole Interval Recording?
- Partial interval says “yes” even if the behavior happened briefly; it inflates time estimates.
- The whole interval requires the behavior to last the full interval; it gives conservative (low) estimates.
- MTS is the middle ground: it samples at moments and is efficient, but it can miss events that occur between moments.
When is Momentary Time Sampling most useful?
Use MTS when:
- You are observing groups (classroom, therapy group), and a single observer can’t track every child continuously.
- Behaviors are high-frequency or occur many times a session, and counting every event is impractical.
- You want a quick trend measure to see whether behavior is increasing or decreasing across sessions.
- You need efficient data during community activities or natural settings where continuous recording is not feasible.
Some practical examples include:
- Measuring how many students are on-task during a 20-minute lesson (one observer can scan the group at each moment).
- Tracking hand-flapping in a classroom where it happens often. MTS gives a workable estimate without nonstop counting.
- Observing engagement at a community outing where staff must also supervise safety.
Benefits of Momentary Time Sampling
- Efficient: Requires less continuous attention than continuous recording, so it works well when observers have multiple responsibilities.
- Good for trends: Repeated MTS sessions quickly show whether a behavior is increasing or decreasing.
- Feasible in groups: One observer can collect data on multiple people by scanning at moments.
- Easy to train: Staff learn to look at specific moments and make a single yes/no judgment; this lowers training time.
- Reduced data volume: Less data to store and analyze than continuous methods, but enough to guide decisions.
Limitations of MTS and How to Reduce Them?
A few common limitations for MTS are as follows:
- MTS misses behavior between moments. If a behavior happens briefly between checks, MTS won’t catch it.
- Variable accuracy depending on interval length. Long intervals reduce accuracy for fast behaviors.
- It results in potential bias. Depending on when the moments fall, MTS can over- or underestimate real occurrence.
How to reduce problems?
- Use short intervals for fast behaviors (15–30 seconds). For slower behaviors, 30–60 seconds can be fine.
- Run pilot sessions comparing MTS with continuous recording on the same behavior to estimate bias.
- Train observers with video practice and use simultaneous IOA checks (aim ≥ 80% agreement).
- Occasional spot-checks with continuous recording help validate your MTS results.
- Interobserver Agreement (IOA) and data quality are essential with any sampling method. For MTS:
Have two observers record at the same moments and compute percent agreement: (agreements ÷ total moments) × 100. Check IOA regularly during training and periodically afterward. If IOA drops, review definitions, timing, and observer procedures, and retrain as needed.
Conclusion
Momentary Time Sampling is a simple, efficient way to collect useful behavioral data when continuous recording isn’t practical. It’s best suited for group settings, busy clinics, and high-frequency behaviors where full-event recording would be too hard. With clear definitions, short intervals, careful observer training, and periodic validation, MTS gives dependable trend data that supports good clinical decisions.
by Raven Health | Nov 14, 2025 | Blogs
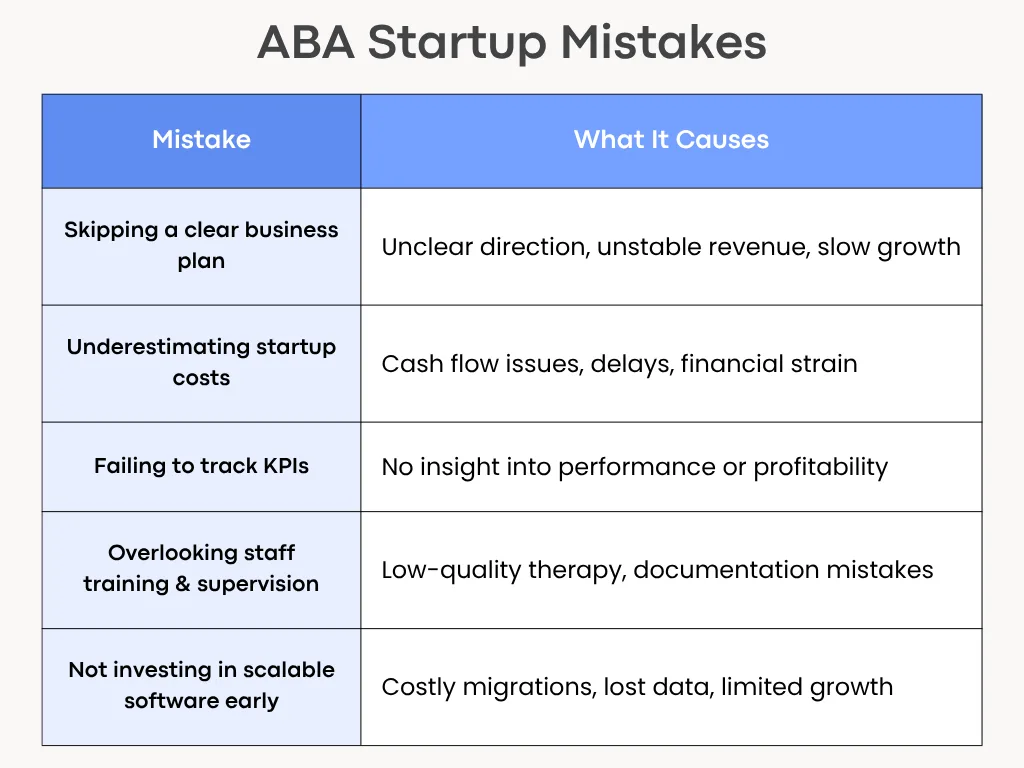
Starting an ABA practice is exciting and full of practical pitfalls. Many new clinics stumble on the same issues that slow growth, hurt cash flow, or risk compliance. In this article, you will explore the most common mistakes that clinics make and practical steps to avoid them.
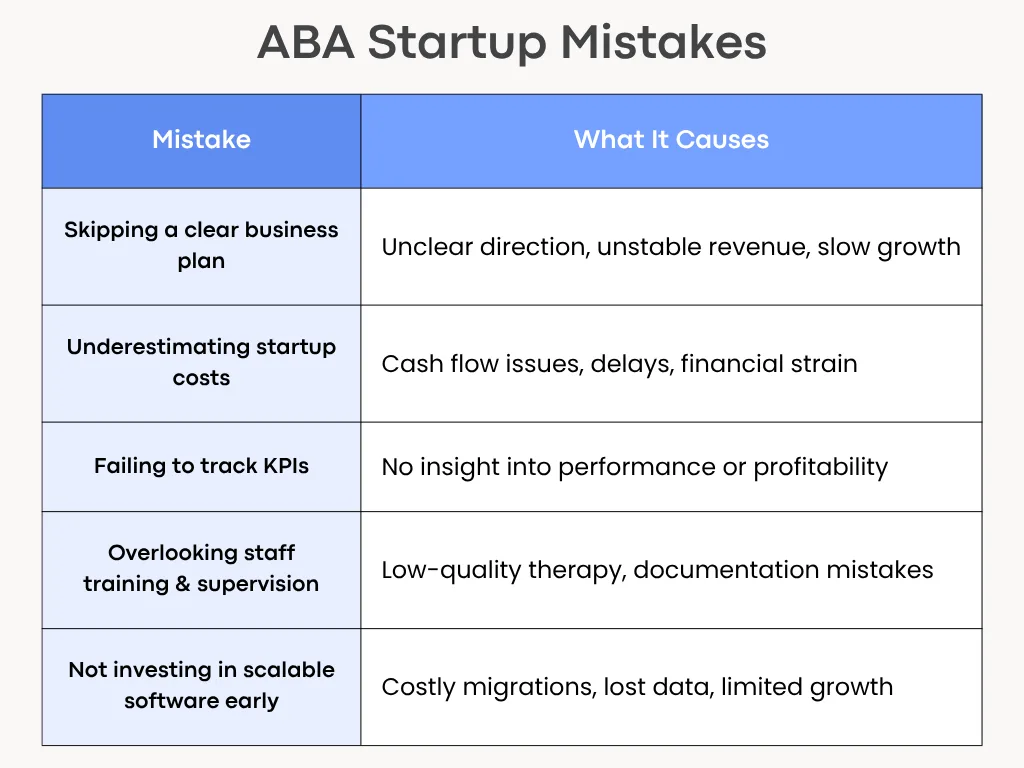
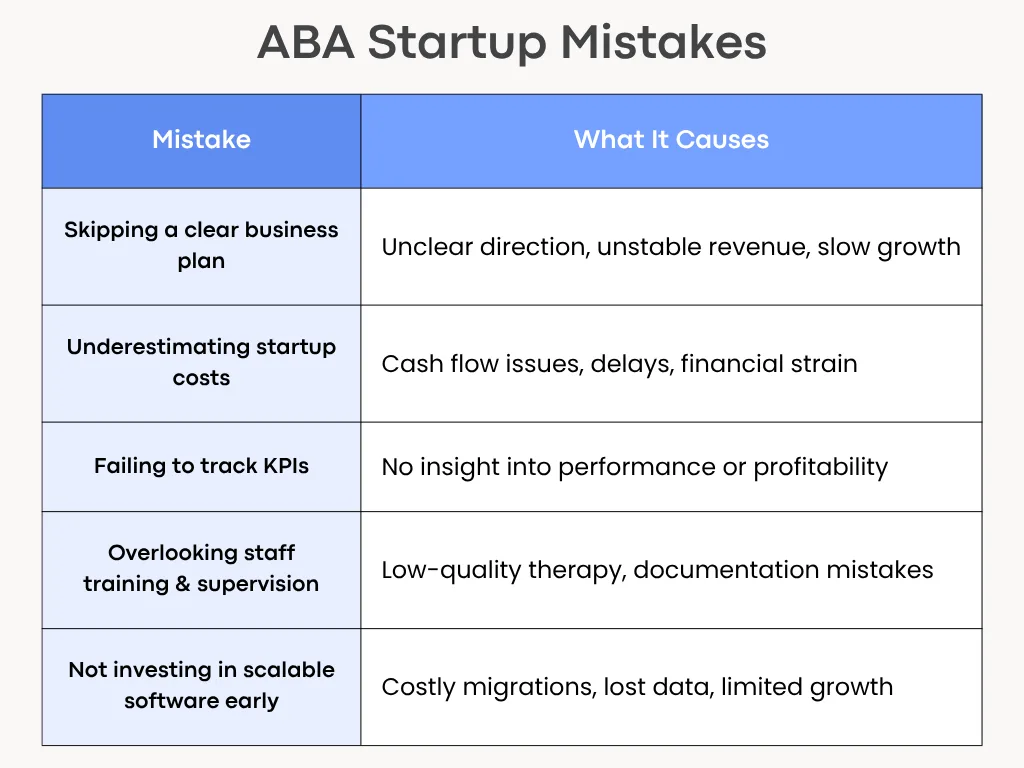
1. Skipping a Clear Business Plan
A good therapy model and strong clinical skills aren’t enough when starting an ABA practice. Without a written business plan, you won’t know who your clients are, how you will get paid, or when the clinic becomes profitable.
What to include in a simple plan?
- Mission and services: Who you serve (age, needs) and which services (intensive ABA, school consultation, tele-health).
- Market and referral sources: schools, pediatricians, insurance panels, and parent groups.
- Revenue model: Typical session rates, payer mix (private pay vs insurance), and expected caseload per clinician.
- Staffing plan: Roles and hires for year 1 and year 2.
- Financial projections: Monthly cash flow forecast for 12 months, break-even date.
- Growth milestones: When to add clinicians, an admin, or a second location.
Write a short one-page plan first and refine it after three months of operations. It’s far easier to adjust a written plan than to improvise under cash pressure.
2. Underestimating Startup Costs
Many founders count only rent and a computer. They miss recurring costs and one-off builds, so cash runs out before the practice stabilizes.
Costs people forget
- Credentialing deposits and payer enrollment fees.
- Billing software, clearinghouse fees, and EMR subscriptions.
- Staff recruitment, background checks, and credential verification.
- Training materials and initial supervision hours for BCBAs.
- Insurance (general liability, professional liability), office supplies, and marketing.
- Working capital to cover payroll for 3–6 months.
Build a conservative budget that includes a three-to-six-month cash buffer. When in doubt, overestimate costs and delay discretionary purchases until revenue is steady.
For more insights, check out our article on ABA startup costs to consider.
3. Delaying Credentialing and Insurance Setup
Credentialing with insurance companies and Medicaid can take months. Waiting to start creates a cash gap and slows patient access.
What to handle early?
- Start payer enrollment as soon as you choose your legal entity and NPI.
- Check state Medicaid requirements and EVV rules if you will bill Medicaid.
- Collect documents up front: provider licenses, malpractice limits, CVs, and contract signatures.
Begin credentialing 90–120 days before you plan to see your first insurance clients. Use a checklist to track submissions and follow-ups weekly.
4. Relying on Paper-Based Data Collection
Paper sheets result in slow supervision, transcription errors, and complicated billing. They also make remote work and audits harder.
Risks of paper
- Lost or illegible session notes.
- Extra admin time to enter data into billing or clinical systems.
- Poor data fidelity for clinical decisions.
Move to a basic digital data-capture tool from day one, even a simple app that syncs to CSV exports. Choose software that supports offline use if you do home visits. Train RBTs on consistent coding and make spot-checks part of supervision.
5. Ignoring Compliance and HIPAA Requirements
HIPAA and state privacy rules are non-negotiable. Gaps expose clients to risk and the clinic to legal and financial trouble.
Key compliance basics
- Sign Business Associate Agreements (BAAs) with any vendor that handles PHI.
- Use encrypted email or a secure portal for families.
- Limit PHI access by role and enable audit logs.
- Keep a breach response plan and test it.
Get BAAs signed before sharing client data. You can use a password manager and MFA for all staff accounts. Also, train staff on privacy rules during onboarding and yearly.
6. Using Disconnected Tools for Billing and Scheduling
Separate systems for scheduling, billing, and charting create manual handoffs, duplicate entry, and missed claims.
Consequences of using disconnected tools
- Billing delays and higher denial rates.
- Frustrated staff who spend time reconciling calendars and notes.
- Hard-to-run reports for utilization or payroll.
Choose an integrated practice management system that fits your budget and workflow. If you can’t afford an all-in-one yet, pick tools with good export/import or API connections and document manual steps to avoid errors.
7. Overlooking Staff Training and Supervision
Good hires aren’t ready without structured onboarding. Undertrained staff make documentation errors and deliver inconsistent therapy.
Elements of strong training
- Role-specific onboarding checklists (RBTs, BCBAs, admin).
- Shadowing and supervised practice blocks before independent caseloads.
- Regular fidelity checks and weekly supervision with documented feedback.
- A clear escalation path for clinical and behavioral emergencies.
Budget for at least 40–80 hours of training per new RBT in the first three months. You can use recorded role-plays and short quizzes to check understanding.
8. Failing to track Key Performance Indicators (KPIs)
Without KPIs you’re guessing whether the business or clinical work is succeeding. Small problems quickly become big.
KPIs to track from day one
- Financial: Days in Accounts Receivable (AR), claim denial rate, net collection rate.
- Clinical: Client attendance rate, average hours per client, and treatment progress by goal.
- Operational: Staff turnover, fill rate for open slots, average time to credential a provider.
Review a short KPI dashboard weekly and a report monthly. Use small experiments (change one thing at a time) and watch the metric move.
9. Neglecting Parent Communication & Collaboration
Parents are partners in therapy. Poor communication hurts retention, progress, and referrals.
What do parents need?
- Clear intake steps and timelines.
- Regular updates: brief weekly notes and a monthly progress snapshot.
- Simple ways to ask questions: portal messages, short phone office hours, or scheduled family meetings.
Send a one-page welcome packet with the treatment plan, goals, who to contact, and what to expect in the first 90 days. Ask for feedback at 30 and 90 days.
10. Not Investing in Scalable Software Early On
Buying the cheapest software that doesn’t scale forces painful migrations later. Data exports, retraining, and process rework cost time and money.
Signs your software won’t scale
- No offline data capture for in-field staff.
- Limited reporting or no API for payroll and billing.
- Difficulty exporting client records in usable formats.
Choose a scalable software like Raven Health that covers core needs (data collection, scheduling, billing, and reporting). Moreover, prioritize exportability and vendor willingness to assist with migration. Consider total cost of ownership, including migration and not just license price.
Conclusion
Many early ABA clinic problems are avoidable with simple, practical planning. Build a short business plan, budget realistically, start credentialing early, and pick scalable digital tools. Train staff well, track key metrics, and keep families part of the process. These steps reduce stress, speed cash flow, and let clinicians focus on what matters most: delivering good care.
by Raven Health | Oct 31, 2025 | Blogs
Good ABA practice management software brings clinical data, scheduling, billing, and compliance into a single system. The right platform cuts paperwork, improves data quality, speeds billing, and helps supervisors make faster clinical decisions. It also supports fieldwork with mobile or offline data capture and provides audit trails for HIPAA and payer rules.
In this article, you will explore the leading ABA practice management solutions and their main features, and differences, so you can choose the best fit with confidence.
What Should ABA Practice Management Software Do?
Good ABA platforms typically include:
- Clinical data collection and program management (trial-level, session-level data).
- Scheduling and staff/credential matching.
- Billing, claims management, and payer rules (including Medicaid/EVV where needed).
- Reporting and dashboards for BCBAs, supervisors, and payers.
- HIPAA-grade security, BAAs, and audit logs.
- Mobile or offline data capture for therapists in the field.
- Training/support and migration help when switching systems.
Look for these features first; the differences between vendors live in how well they do each item.
Leading ABA Platforms
1. Raven Health
Raven Health is built for new and growing ABA practices that value simplicity, speed, and an intuitive user experience. Designed with both clinical and operational efficiency in mind, it brings data collection, scheduling, and billing together in one seamless platform.
Features: Raven Health offers a simple user interface with drag-and-drop scheduling feature that simplifies coordination across teams. It’s designed for RBTs in the field who need reliable offline data entry. The platform also includes AI-generated session notes to help clinicians save time while maintaining accuracy and compliance. For billing, teams can choose Managed Billing services for full revenue cycle support—ideal for practices that want to minimize administrative work and focus on care.
Best for: Startups and Small-to-medium ABA clinics seeking an affordable, all-in-one platform with seamless onboarding and integrated billing.
2. CentralReach
CentralReach is a full practice management software that connects clinical data, scheduling, claims, payroll, and analytics in one system. It’s widely used by larger clinics and multi-site organizations.
Features: It offers program books that sync with data sheets, automated clinical reports, payroll and claims integration, and outcomes/analytics dashboards. Field therapists can collect data offline and sync later, which helps home-based programs and community sessions.
Moreover, built-in payer rules, claims scrubbing, and automated workflows reduce denials and speed payment cycles for larger practices. Dashboards for outcomes and productivity help supervisors track program fidelity and clinic KPIs.
Useful AI features are appearing in recent releases for session summaries and analytics.
Best for: Growing practices or multi-site organizations that need advanced billing and large-scale reporting.
3. Rethink Behavioral Health
Rethink combines clinical programming and staff training with core practice management features. It aims to reduce onboarding time by bundling curriculum content with data tools and scheduling.
Features: It offers built-in curricula and training where you can find integrated clinical content (curriculum library and embedded training), built-in videos for staff training, dashboards, and payer-ready reporting. Rethink also supports scheduling across locations and can include EVV features where required.
Core practice management functions are included so smaller clinics can use one vendor for both clinical content and operations. Rethink is a strong resource hub for clinical best practices and team development.
Best for: Clinics that want an “out-of-the-box” curriculum plus practice management in a single vendor.
4. Notable
Noteable positions itself as an all-in-one EHR and practice platform for behavioral health and ABA. It emphasizes streamlined workflows, billing, and analytics
Features: It has a broad EHR/practice management feature set with particular focus on billing and revenue management, scheduling, documentation, automated billing/RCM options, tele-health, and supervision workflows.
It offers client portals and integrations for multi-program organizations. Screen sharing, supervision mode, and remote signatures support BCBA oversight and remote work.
Best for: Clinics that need strong billing/RMC support alongside clinical data collection.
5. AlohaABA
AlohaABA is built for ABA operations and highlights authorization tracking, payroll, billing, and EMR features tailored to ABA workflows.
Features: As said, it is built specifically for ABA, with tools for authorization & AR management to track referrals, accounts receivable, compliance validation, consolidated reports, and analytics tailored to ABA billing rhythms.
It offers business insights by providing reports focused on utilization, staff productivity, and revenue metrics that managers use to run clinics.
Best for: Medium practices that want ABA-focused business workflows and strong operational reporting.
6. Ensora Health
TheraNest (now under Ensora product family for mental health) is not ABA-specific but is widely used by small therapy practices. It’s affordable and covers scheduling, notes, billing, and tele-health
Features: It offers the client portal, tele-health, flexible templates, scheduling, notes, and good small-practice support. TheraNest is not ABA-specific but works well when clinics can adapt templates for ABA use.
Best for: Solo practitioners and very small clinics who want an inexpensive, flexible EHR and can adapt templates for ABA.
How do these Platforms Help Clinics?
1. Save Clinician Time
Automated graphs, session note drafts, and synced program books mean less manual charting and faster supervision reviews. CentralReach emphasizes automatic reporting tied to session data.
2. Reduce Billing Errors and Speed Revenue
Platforms with built-in payer rules, claims scrubbing, and RCM workflows shorten claim-to-payment cycles (Noteable and CentralReach emphasize RCM and claims tools).
3. Improve Clinical Decisions
Real-time dashboards and fidelity checks (program adherence, staff performance) give BCBAs the data to adjust programs faster. Vendors like Raven and Rethink highlight dashboards and analytics for clinical oversight.
4. Support Compliance
HIPAA, audit trails, EVV where required, and account/credential flagging are built into several platforms to reduce compliance risk.

How to Pick the Best Fit for Your Clinic?
Managing both clinical care and complex business tasks is an essential part of running an ABA clinic.
- Start with your biggest pain point**.** Is it billing? Scheduling? Data fidelity? Pick the vendor that fixes that first.
- Match product to practice size. Enterprise platforms for multi-site growth (CentralReach); simpler, faster, low-cost options for startups (Raven).
- Ask about compliance and BAAs. Get written confirmation on HIPAA, encryption, and whether the vendor will sign a BAA.
- Test mobile workflows. Have an RBT do a trial session on the vendor app (data entry, offline sync, speed).
- Request references of similar-sized practices. Ask how long onboarding took and how the vendor handled data migration.
- Check billing outcomes. If revenue cycle matters, ask for average claim acceptance rates, denial reduction examples, or RCM case studies. (Vendors offering RCM or billing services will usually have these numbers.)
- Pilot before committing. Run a short pilot with a small caseload to validate reporting, staff buy-in, and integration points.
Final Thoughts
Choosing the right ABA practice management software is a strategic decision. The right platform centralizes clinical work, reduces administrative burden, and helps your team make better, faster decisions. No single product fits every clinic; the best choice depends on your size, priorities, billing complexity, and how much you value clinical depth versus operational features.

by Raven Health | Oct 30, 2025 | Blogs

Artificial intelligence (AI) is changing how ABA clinics run day to day. In practice management, AI tools can speed up routine tasks like writing session notes, spotting patterns in behavior data, scheduling appointments, and producing clear reports. That frees clinicians to spend more time on treatment and supervision, while making operations smoother and more predictable.
In this article, you will explore the real ways AI is already helping ABA providers, the important safeguards clinics must keep in place, and a practical view of where AI can add value and what to watch for when bringing these tools into your practice.
How AI helps ABA Practices?
AI is not a replacement for therapists. It’s a set of tools that automates repetitive work and highlights signals humans should act on. Key areas where AI adds value are as follows:
1. Automatic Transcription
AI can transcribe session audio into text so clinicians spend less time typing notes. Some clinics use AI tools for ABA that automatically link these transcripts to client profiles, reducing manual uploads and improving data consistency.
2. Drafting Structured Notes
After a session, AI can propose a draft progress note or a summary of target behaviors, leaving the clinician to edit and sign. That cuts paperwork time while keeping the clinician in control of clinical content.
3. Pattern Spotting
AI can scan months of session data and flag trends such as rises or drops in specific behaviors that might be hard to see by hand. This supports faster clinical decisions.
4. Predictive Signals
Models can suggest which clients may respond to a given strategy or when a behavior is likely to escalate, helping teams plan proactively. Use these signals as prompts for human review, not final decisions.
5. Smart Scheduling
AI tools predict demand, suggest optimal appointment times, and automatically offer slots to families, reducing back-and-forth scheduling. Some systems report meaningful drops in no-shows and better daily workflows.
6. Reminders and Triage
Automated reminders, pre-visit checklists, and conversational bots can handle routine communications so staff can focus on care.
7. Cleaner Datasets
AI helps standardize and clean raw data so reports show consistent fields and units. That reduces errors that creep into manual data entry.
8. Faster Reports
Generate visual progress charts and exportable summaries for insurance, supervision, or team meetings with much less manual work.
Important Considerations Before Adopting AI
AI has upside, but clinics must be deliberate. Here are the core concerns and how to address them.
Privacy and HIPAA compliance
Any AI that accesses protected health information (PHI) must be treated under HIPAA rules. That means encryption, strict access controls, BAAs (Business Associate Agreements), and careful logging of who saw what. Do not assume a vendor’s marketing line is compliance; verify contracts and technical measures.
Ethics and bias
AI models can reflect the biases in their training data. That can skew predictions about which clients may succeed or fail with a strategy. Vet models for fairness and test them on your own data before relying on outputs.
Transparency and explainability
Prefer tools that show how they reach recommendations (features they used, confidence levels). If a system makes a surprising call, like flagging a client for urgent review, clinicians must be able to inspect why. Opaque “black box” decisions are risky in clinical care.
Human judgment remains essential
AI as support, not authority: Use AI outputs to focus clinician attention. Final clinical decisions, treatment planning, and ethical judgments must rest with trained humans. AI can speed up work—never replace clinical reasoning.
Practical Rollout Checklist for Clinics
Before you switch on an AI feature, run through this list:
- Define the use case. Start with one problem: note automation, schedule optimization, or a data-flagging dashboard.
- Vendor vetting. Ask for security docs, SOC 2 or similar attestations, HIPAA compliance proof, and whether the vendor signs a BAA.
- Data governance. Decide what data will be shared, how long it’s kept, who can access it, and how to remove it if needed.
- Bias and testing. Test the tool on historical, de-identified clinic data. Check for strange or biased outputs.
- Explainability requirement. Prefer tools that provide rationale or confidence scores with each recommendation.
- User training. Teach staff how to interpret AI outputs and how to spot errors. Include clear escalation routes.
- Consent and transparency. Let families know what AI tools the clinic uses and how data is protected. Obtain any consent required by policy.
- Monitor and review. Set metrics for success (time saved, decreased no-shows, report accuracy) and review outcomes regularly.
Risks to Watch and How to Reduce Them
- Over-reliance– Never let AI outputs override clinical checks. Always require a clinician’s sign-off.
- Data leaks- Limit exported data and apply strict identity access controls. Log accesses and run audits.
- Model drift- AI models can degrade as clinic populations change. Retrain or revalidate models periodically.
- Regulatory change– Keep legal counsel involved because the rules for AI in healthcare are evolving fast. Stay current with guidance from regulators and trusted health IT sources.
Final Thoughts
AI can make ABA practice management faster and clearer. It reduces routine paperwork, surfaces meaningful patterns, and helps clinics use staff time where it matters most. At the same time, privacy protections, ethical safeguards, and human oversight are non-negotiable. Start small, test thoroughly, and keep clinicians at the center of every workflow change. That combination of smart tools and human judgment offers the best path to safer, more efficient ABA services.
by Raven Health | Oct 28, 2025 | Blogs
Continuous measurement is a data‑collection method in Applied Behavior Analysis where every occurrence of a target behavior is recorded during a set period. In simple terms, this means an ABA therapist (such as a BCBA or RBT) notes each time the behavior happens. For example, counting every time a child raises their hand or timing the length of a tantrum.
In this article, you will explore the difference between continuous measurement and discontinuous methods, the main techniques used in continuous measurement, and its significance for accurate data collection and progress tracking.
What is Continuous Measurement in ABA?
Applied Behavior Analysis relies on careful data collection to track and change behavior. Continuous measurement means recording every occurrence of a target behavior during an observation period. For example, with continuous recording, a therapist would note all of a student’s temper tantrums during a session. Thus, continuous recording gives a full, detailed account of the behavior.
This thorough tracking helps therapists see patterns and evaluate progress: it provides a detailed and comprehensive view of what’s happening and ensures that no instances are overlooked. In other words, continuous data gives ABA teams the accurate, reliable information they need to make informed treatment decisions.
Continuous vs. Discontinuous Measurement
The choice between continuous and discontinuous methods depends on the situation and behavior. Continuous methods produce the most accurate data because nothing is missed. However, they require more time and attention.
Discontinuous measurement (like partial or whole interval recording) is less demanding but only gives approximate data. In practice, ABA professionals select the method that best fits the behavior and resources.
For example, if you need a complete record of every occurrence (such as during an initial assessment or when behaviors are quick and frequent), continuous measurement is preferred.
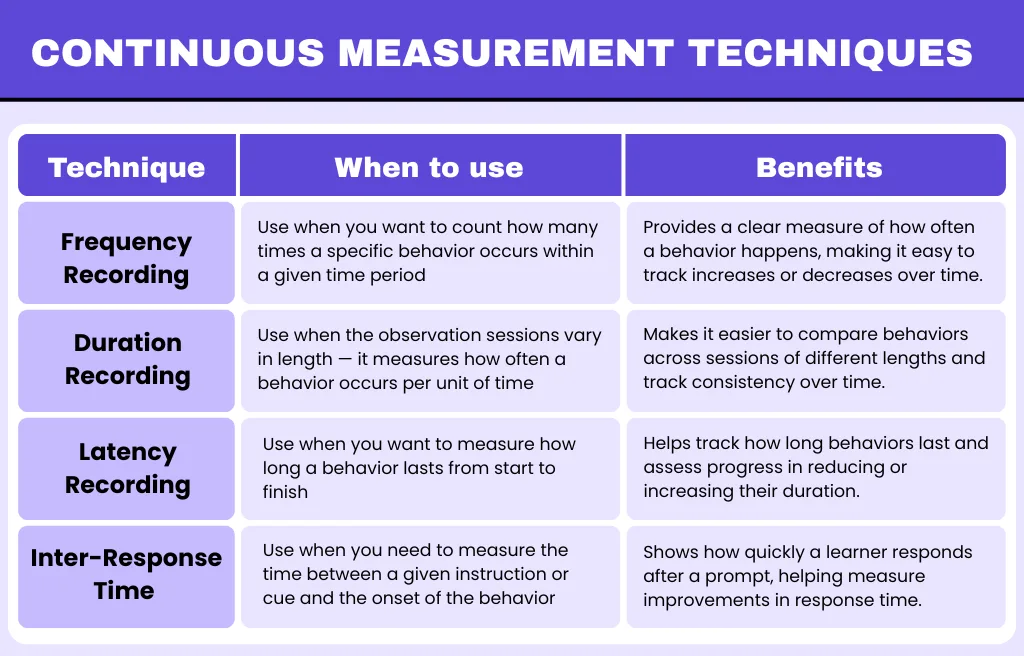
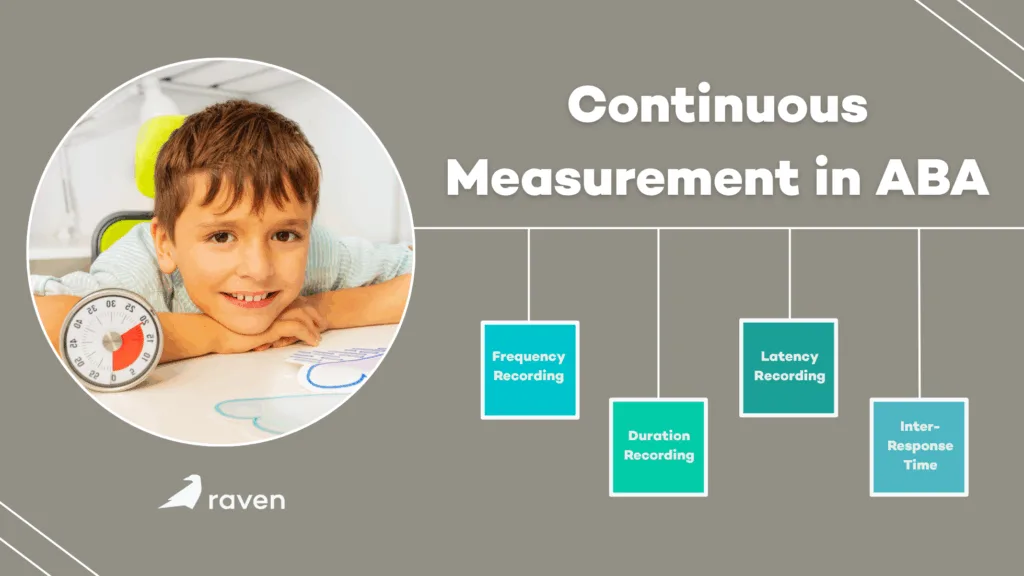
Continuous Measurement Techniques
Several specific techniques fall under continuous measurement. Each tracks behavior in a different way:
1. Frequency (Event Recording)
Frequency measurement simply counts how many times a behavior happens. The observer tallies each occurrence during a session (using marks, counters, or beads). This is useful when the behavior has a clear beginning and end, such as raising a hand or throwing a toy.
For example, if you want to know how often a child raises their hand to answer questions, you would record each hand raise as it occurs. Frequency data are easy to collect and analyze, and they give a straightforward measure of how often a behavior occurs.
When to use frequency: Discrete, countable behaviors with clear starts and stops (i.e., number of questions asked, times out of seat). Record each instance as it happens.
Benefits: Simple and direct; shows exact count of behavior occurrences.
Limitation: Does not account for how long each instance lasts, and on its own can be misleading if session lengths vary greatly.
2. Duration Recording
Duration measurement records how long each instance of a behavior lasts from start to finish. The observer uses a stopwatch or timer to measure the length of each occurrence. This technique is ideal for behaviors where total time matters, such as tantrums, time spent on-task, or any continuous activity.
For example, a therapist might time how long a student stays focused on a task or how many seconds a tantrum lasts. By capturing the duration, practitioners can see not just how often the behavior happens, but how long each episode is.
When to use duration: Behaviors with indefinite length or no clear countable instances (i.e., time spent in tantrum, continuous hitting). Use when you want the total time measured.
Benefits: Provides insight into intensity or severity (longer durations may indicate more severe behavior).
Limitation: Requires watching behavior continuously to time start and end; can be difficult if multiple behaviors overlap.
3. Latency Recording
Latency measures the time between a prompt (or signal) and the start of the behavior. In practice, you start a timer when you give a cue (like an instruction or signal) and stop it when the person begins to respond. Latency is useful for evaluating response speed.
For example, if a teacher asks a question and the student takes 5 seconds to start answering, those 5 seconds are the latency. This helps practitioners know if responses are too slow or if they occur too quickly, and adjust teaching strategies accordingly.
When to use latency: When the timing of a response is important (i.e., time from instruction to beginning of task). Useful in teaching programs where you want to decrease response delay.
Benefits: Pinpoints reaction time, helping track improvements in response speed or identify delays.
Limitation: Only captures the first response after each prompt, so it’s not useful for behaviors that happen without a clear cue.
4. Inter-Response Time (IRT)
Inter-response Time (IRT) measures the time between consecutive occurrences of the same behavior. It is the interval from the end of one instance until the start of the next. This shows how quickly a person repeats a behavior.
For example, IRT might be used to measure the time between bites during a meal or between questions asked by a student. Short IRT means the behavior is happening frequently (rapid pace), while long IRT indicates slower occurrence.
A behavior analyst might use IRT to speed up a desired behavior (by decreasing IRT) or to slow down an undesired one (by increasing IRT).
When to use IRT: When the pattern of repeated behavior is of interest (i.e., how much time passes between consecutive problems solved or between episodes of a behavior).
Benefits: Highlights the pacing of behavior, useful for tasks that involve multiple steps or repeated actions.
Limitation: Requires a clear end of one response and start of the next; not applicable if behaviors don’t occur in sequences.
Importance of Continuous Measurement
Continuous data are valued because they give the clearest and most precise picture of behavior. By capturing every instance, continuous measurement methods produce the most accurate data.
This comprehensive recording means analysts don’t miss rare or brief occurrences, which can be overlooked by sampling methods. As a result, continuous measurement allows practitioners to see detailed trends.
With continuous data, therapists can track exactly how a behavior changes over time and in response to intervention. For example, a therapist can plot each session’s total occurrences and see if an intervention is reducing the behavior. This level of detail is crucial for evaluating if goals are being met.
In fact, continuous tracking often yields more reliable progress monitoring; it helps ABA professionals assess whether a treatment plan is working and make timely adjustments.
Since continuous recording collects all data, it reduces bias and ensures that even subtle improvements or worsening of behavior are noticed. For these reasons, continuous measurement is preferred when accuracy is critical, such as during initial assessments or when closely monitoring an intervention’s effects.
When Is Continuous Measurement Preferred?
Continuous measurement is best suited to situations where a full record of behavior is important. For example:
High-Frequency Behaviors
When a behavior happens often (i.e., a student raising their hand many times in class), continuous recording captures each instance. This gives an accurate count of how engaged the student is.
Long-Duration Behaviors
For behaviors that last a while (like a tantrum or extended on-task work), continuous measurement tracks exactly how long each episode lasts. Knowing the duration is key to understanding severity or focus level.
Precise, Data-Driven Decisions
In early stages of therapy or research, clinicians use continuous tracking to establish detailed baselines. By establishing clear goals based on documented behaviors and observing every occurrence, therapists can monitor progress accurately and adjust plans in real time.
One-on-One Settings
When a therapist works with one person (so full attention is possible), continuous methods are practical even for relatively rare behaviors. Capturing each instance (even if infrequent) provides a complete picture, which can be vital when tailoring interventions.
Conclusion
Continuous measurement is the method of choice when you need exact data on how often or how long a behavior occurs. It is most practical for discrete, countable behaviors and for capturing the full extent of an action. When used appropriately, continuous data collection lets ABA professionals track changes and progress with confidence, ensuring interventions are based on solid evidence.